It is time to sleep Better and Cheaper
At Mattressnut we understand how overwhelming it can be to find a new mattress or bedding product with so many brands on the market nowadays. But no worries, we are here to help you in your quest.
Because a good night of sleep is so important
Great quality bedding products accessible for everyone
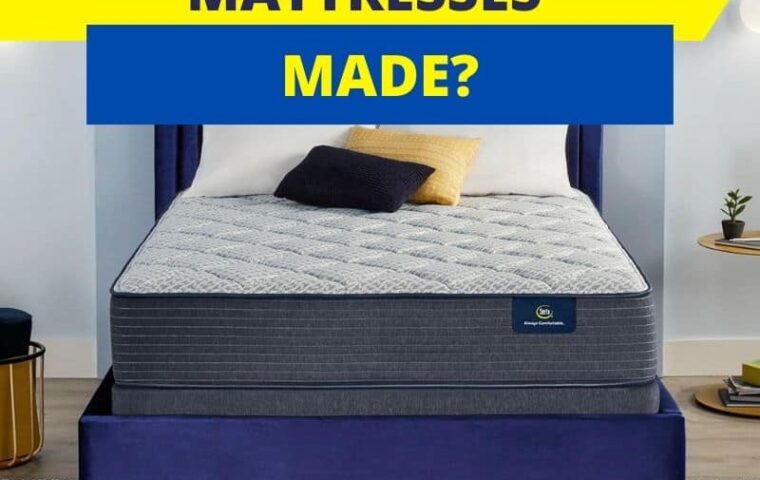
We source and review various bedding products (mattresses, pillows, bed foundation, bunk beds etc) to help you find the perfect fit for your needs.
We work closely with brands to get you the best deals
We do our best to select product for every budget and needs
On the heavy side
5 nice bed frames for heavy people | Our top 10 mattresses for heavy person | 5 mattresses options for 300 pounds people | 10 picks for a 400 pounds person
By foundation type
10 mattresses for adjustable base | Choose a mattress for a murphy bed | Bed frames for a memory foam mattress | High rise bed frames | 5 amazing low profile box spring | Foundation for an hybrid mattress | Top 10 mattresses for a platform bed
For organic lovers

10 best organic mattresses | Organic toddler pillows | Our 5 favorite organic mattress toppers | Top 10 organic pillows | 5 great cotton mattresses we love | 5 copper infused mattresses we recommend | Organic pregnancy pillows
Bed Sheets options

10 bed sheets for winter | Bed sheet set for an adjustable base | Our pick for airbnb bed sheets | Best sheets for dorm | 10 bed sheets for a memory foam mattress | Best sheets for the summer | 5 bed sheets for allergy | Our top bed sheets with pockets
By mattress type

Our favorite flippable mattresses on the market | 5 great latex free mattresses | Top 10 mattresses for sex | Best mattresses for athletes | Mattresses for combination sleepers | Top mattresses without box spring | Best fiberglass free mattresses